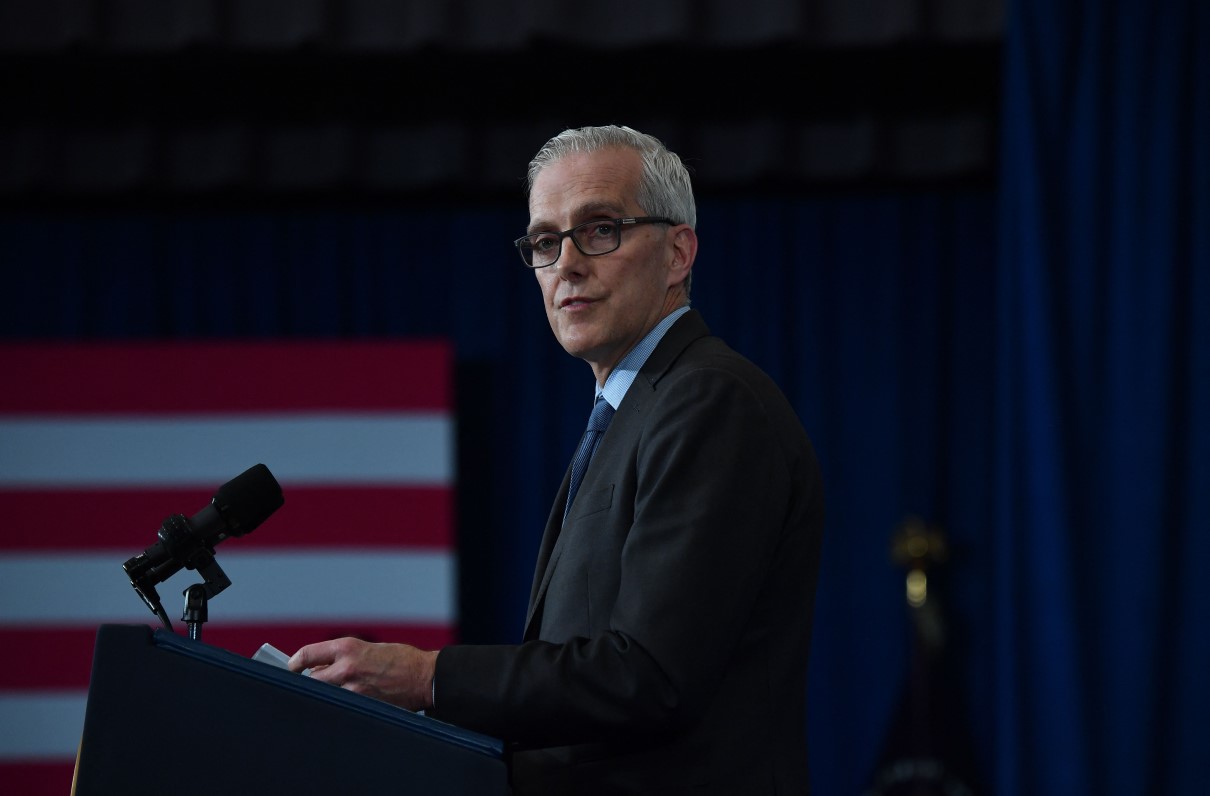
“This budget delivers critical resources to help VA serve veterans, their families, caregivers, and survivors as well as they have served this country,” Secretary of Veterans Affairs Denis McDonough said in a press release announcing the budget, “and it will allow VA to continue providing more care, more services, and more benefits to more veterans than any time in history.”
The proposed topline budget of more than $300 billion reflects a growth trend across the enterprise dating back to 1995, when the VA was funded at only $37 billion. The rate of growth between veterans’ health care and benefits spending has remained similar over the years, even with rapidly rising health care costs across the country.
The FY 2023 budget requests over $139 billion in discretionary funding, the majority of which is for health care. The Veterans Health Administration’s (VHA) budget is a little over 41% of VA’s total budget and covers medical services, medical community care, staffing, facilities, and other technology and administrative costs. About 9.2 million veterans are enrolled in VA health care, although only two-thirds use the VHA health system.
[RELATED: Get an In-Depth Look at MOAA’s Veteran Health Care Priorities]
The administration has also requested a little over $132 billion in FY 2024 advanced appropriations for medical care – a 7.7% increase over 2023. Advanced appropriations provide continuity of health care between fiscal years in the event of a government shutdown or other situation that prevents funding of annual budgets.
A large segment of health care spending in recent years is a result of the VA MISSION Act, enacted in 2018 to modernize and expand veterans’ access to health care services within the VA direct care system and through its community care provider network. The VHA budget has increased $104 billion, or 53%, since the act became law.
Other factors driving up medical costs in this year’s budget proposal include projected sector-wide health care inflation, along with increased veteran enrollments and demand for care. The pandemic has caused many veterans to delay their care; with COVID-19 cases declining in the U.S., the VHA expects high pent-up demand for routine and specialty care. It also expects the health impacts of the pandemic on veterans to be longer lasting.
VA Budget Proposal vs. MOAA’s Priorities
MOAA is grateful to the administration and the VA for their commitment to serving veterans and for reflecting many of our priorities in the budget request. Here is how that request addresses some of MOAA’s key issues.
1. Prioritizing and accelerating access to caregiving support, as well as long-term and extended care programs and services.
The VA covers a spectrum of geriatric, extended care, and caregiver support services in a variety institutional and non-institutional settings. Many veterans prefer living at home as long as possible. The VA also provides a range of home- and community-based long-term care programs to meet veterans’ needs over time.
The department is requesting over $20 million for institutional VA and community nursing home care, and another almost $16 million for non-institutional care like adult day health care, telehealth, home-based primary care, purchased skilled home care, and other services. Some of the proposed funding covers VHA’s expansion of existing long-term extended care and other geriatric programs like palliative and hospice care.
Another $1.8 billion is proposed for VHA’s Caregivers Support program, which includes the Program of General Caregiver Support Services and the Program of Comprehensive Assistance for Family Caregivers (PCAFC). The figure reflects a $433 million increase from FY 2022.
[RELATED: Check Out MOAA’s Updated Caregiver Resources]
The PCAFC has been fraught with problems since expansion of the program was congressionally mandated in the MISSION Act. Long delays in implementation, high denial rates, and lack of consistency in how the VA is implementing the regulations have resulted in a number of pauses in program operations.
The March 23 pause prevented thousands of caregivers and their veterans from being terminated from the program and losing their health care and stipend payments. The VA will continue providing benefits to caregivers and resources during the moratorium. The budget proposal provides the VA with the resources to continue assessing legacy applications and processing new applications.
Funding also covers the program’s expansion – it’s now open to those who joined service before May 7, 1975, and to those who joined after Sept. 11, 2001, with plans to incorporate those who served between those dates beginning Oct. 1 of this year.
2. Eliminating disparities faced by women, minority, and underserved veterans, and expanding access and services to ensure equitable delivery of health and benefits among all veteran populations.
The number of women veterans using VA services has more than tripled since 2001 – from 159,810 to over 600,000 – and will continue to grow in the coming years. MOAA has pressed the VA and Congress to ensure women, minority, and underserved veterans have access to timely, high quality, specialized health care services to the same extent as their peers. The department also must provide a safe, welcoming, and harassment-free environment at all its health care facilities.
Though specifics on health care for this segment of the veteran population are not broken out in the VA’s budget request, the department has indicated it is increasing all women’s health care by $9.8 billion, up $756 million from FY 2022. VHA expects to spend about $767 million in support of gender-specific care and women’s health programs.
The proposal “supports investments in comprehensive specialty medical and surgical services for women veterans,” according to the budget document, and would “increase access to infertility counseling and assisted reproductive technology (ART) and to eliminate copayments for contraceptive coverage.”
The ART provisions, including in vitro fertilization and adaption reimbursements, and copays for contraception-related health care services will require Congress to provide the VA the legislative authority for the reproductive technology changes.
The VA has also committed to ensuring sufficient funding for prosthetic research specifically for women veterans and implementing a zero-tolerance policy for sexual harassment and assault at VA facilities.
[RELATED: Big Step for Bill Increasing Veterans’ Access to Breast Cancer Screening]
3. Ensuring the VA continues executing enacted legislation to improve access and delivery of behavioral health and suicide prevention services.
MOAA is encouraged by the VA’s commitment to keeping veterans’ mental health and suicide prevention programs and services a top priority as indicated in its budget submission.
The administration has taken a government-wide approach in increasing health care access and lowering costs, with initiatives outlined in budget request from the VA, DoD, and Department of Health and Human Services. The VA is requesting $13.9 billion for improvements and increased access to mental health care services, and is seeking legislative change to lower veterans’ out-of-pocket costs for that care.
The department is also requesting $497 million to implement grants for community-based suicide prevention efforts and funding to transition to a new 988 universal telephone number for a National Suicide Prevention Lifeline to be implemented later this year. Another $663 million is to support opioid and substance abuse prevention and treatment programs, and $2.7 billion is set to fund for homeless programs, which include access to high-quality health care and services to prevent and end veteran homelessness.
4. Stabilizing and modernizing the VHA health care workforce and support systems.
Sustainment of VHA’s workforce and modernizing its human resource policies and practices has long been of concern to MOAA.
Medical staff are the backbone of the VA health system. Surveys continue to show veterans prefer their care from the VA, with trust in the system on the rise. MOAA believes it is essential our country prioritizes its investment in VA health care in support of its foundational missions — clinical, education, research, and national emergency response.
[RELATED: What Does the VA Facility Realignment Plan Mean for Veterans’ Health Care?]
This too is a priority for Secretary McDonough -- he announced a Human Infrastructure plan Feb. 9 outlining the importance and urgency of investing in VA’s workforce and plans for making the department a model employer where employees will want to work.
The VA’s budget submission reflects growth in VHA and human resource staff and services to support personnel recruiting, retention, and personnel support programs. The budget request supports the recent passage of the VA Nurse and Physician Assistance RAISE Act included in the Consolidated Appropriations Act and signed into law on March 15 to fund the federal government for this fiscal year. The provision will provide pay raises for advanced practice registered nurses and physician assistants at the VA. Lifting the existing pay cap for these positions will help the VA remain competitive with other health care systems.
MOAA has urged current and future secretaries to commit to carrying out the plan, and has sought congressional support for investing in employees’ wages and other workforce incentives outlined in the secretary’s plan.
Other Priorities
It is difficult to assess how the budget will address other MOAA priorities of predictable funding for the VA and oversight and accountability for the department. However, VA’s FY 2022-28 Strategic Plan, released at the same time as its budget request, highlights four strategic goals that attempt to address MOAA priorities. The plan states the VA will:
- “Consistently communicate with our customers and partners to assess and maximize performance, evaluate needs and build long-term relationships and trust.”
- “Deliver timely, accessible, high-quality benefits, care and services to meet the unique needs of veterans and all those we serve.”
- “Build and maintain trust with veterans, their families, caregivers and survivors — as well as employees and partners — through proven stewardship, transparency and accountability.”
- “Strive toward excellence in business operations — including governance, systems, data and management — to improve experiences, satisfaction rates, accountability and security for veterans.”
More details on the VA’s health care budget are expected in the coming weeks as the department releases additional information and VA officials provide their rationale in upcoming hearing with the House and Senate veterans’ committees.
More Members Mean More Influence Over Our Health Care
Get involved and make sure your interests are addressed. Because the larger our voice is, the greater our impact will be.