 Editor’s Note: This article is part of MOAA’s 2023-24 TRICARE Guide, brought to you by MOAA Insurance Plans, administered by Association Member Benefits Advisors (AMBA). A version of the guide appeared in the November 2023 issue of Military Officer magazine.
Editor’s Note: This article is part of MOAA’s 2023-24 TRICARE Guide, brought to you by MOAA Insurance Plans, administered by Association Member Benefits Advisors (AMBA). A version of the guide appeared in the November 2023 issue of Military Officer magazine.
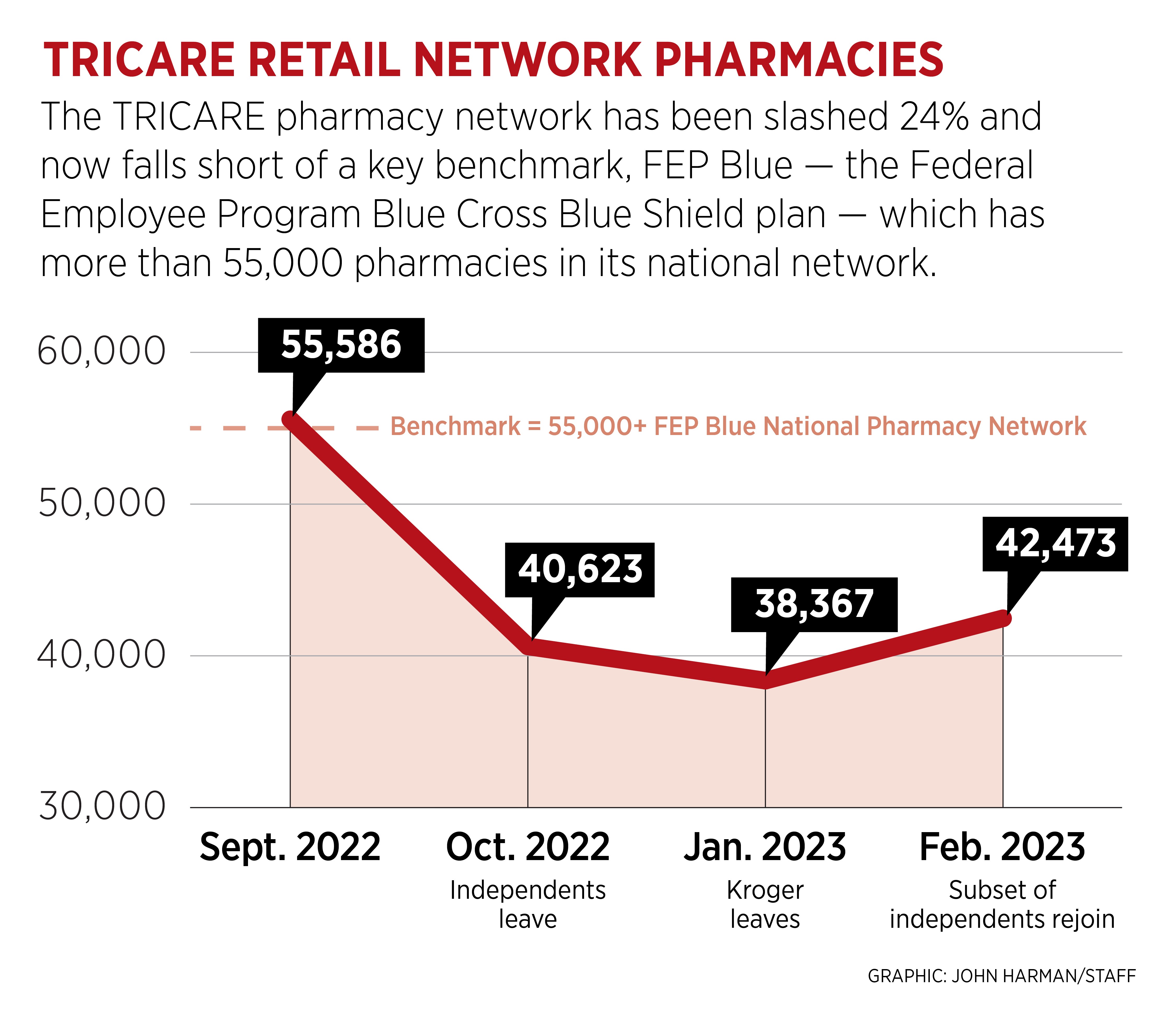
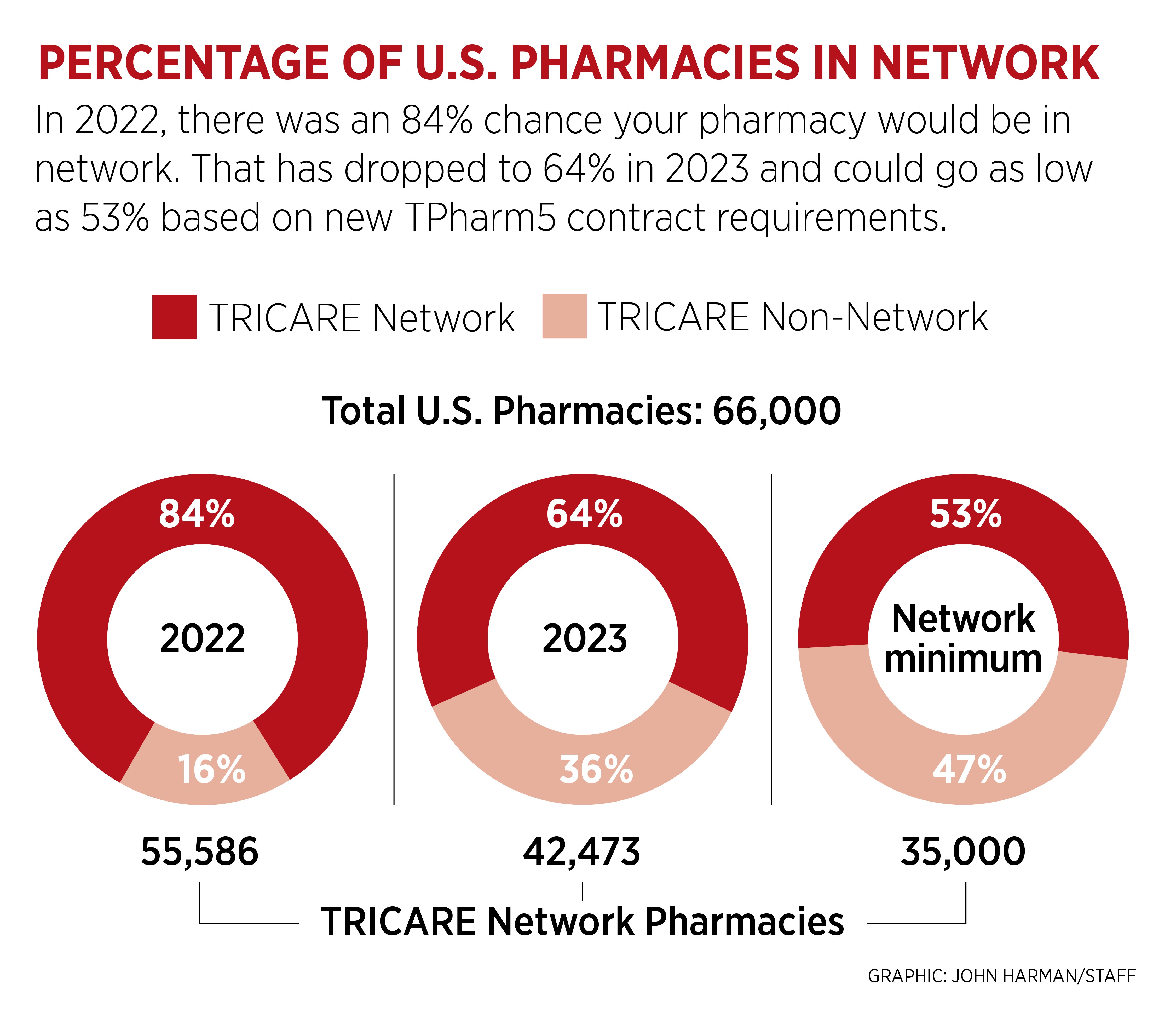
You should care about TRICARE pharmacy network cuts even if they don’t affect you. With the transition to the new TRICARE pharmacy contract, the retail pharmacy network was slashed by nearly 25% as thousands of independent pharmacies and the Kroger family of stores left the network due to reimbursement rates that reportedly wouldn’t even cover their costs.
Chances are, you won’t be affected by this change. Only a small percentage of TRICARE beneficiaries have filled a prescription at one of the departing pharmacies in the past six months — so why should you care?
[TAKE ACTION: Ask Your Lawmakers to Preserve the TRICARE Pharmacy Benefit]
This network reduction is a cut to the military health care benefit, earned through service and sacrifice, and sends a clear message: The TRICARE coverage you are counting on is at risk. The reduced pharmacy network decreases choices and options for all TRICARE beneficiaries. If you are in the fortunate majority of healthy families, it likely won’t be a problem to switch to another network pharmacy for your occasional medication needs, but pharmacy options matter to many military families.
Options matter to the elderly. Seniors often have limited transportation as well as mobility, vision, or hearing challenges and depend on enhanced services provided by community pharmacies.
Options matter for rural residents. Many rural areas lack large chain stores. Families in rural areas depend on community pharmacies, and now military families and retirees must drive past their local pharmacies and/or Walmart, then many more miles to get to a network pharmacy.
Options matter after a hospitalization. Many of the pharmacies no longer in the network are located in hospital lobbies or other medical settings — locations that make it easier for patients to get their medications during challenging situations.
[TRICARE GUIDE: Moving to Medicare at 65 and Over]
Options matter during drug shortages. Problems with the prescription drug supply chain are becoming more common. A narrowed network means fewer possibilities to find the drug you need in network.
Options matter after a devastating diagnosis or when you need an uncommon drug. MOAA members report independent pharmacies are more willing than large chains to special order medications they don’t typically stock.
Options matter for long-term care residents. Assisted-living facilities use a single pharmacy that supplies all residents with specially packaged prescriptions to reduce medication administration errors. A robust network increases the chances your long-term care pharmacy is in network. Otherwise, as many frantic families have learned, you’ll have to pay 100% out of pocket for your medications and file a claim for partial reimbursement.
Military families’ pharmacy options today are dramatically reduced from those available over the past 20 years of the program, when the network had no fewer than 50,000 retail locations.
These pharmacy cuts might not impact you directly, but they send a message to every military family: Your TRICARE benefit is at risk.
[TRICARE GUIDE: Here’s How You Can Help MOAA Protect TRICARE and TRICARE For Life]
What version of TRICARE do you want in place when you need it? The low-cost, robust, quality coverage/access version that existed for 20 years — while many of you were serving multiple combat deployments — or a whittled-down version that fails your family when you need it most?
MOAA has spent the past year raising awareness of this issue and advocating for a report to evaluate beneficiary impact of the pharmacy network cut. These efforts have achieved language in both the House and Senate versions of the FY 2024 National Defense Authorization Act. MOAA is working to ensure a report requirement is included in the final version of the bill. The findings from this report will drive our future advocacy efforts.
What can you do?
- Contact your lawmakers and tell them cutting TRICARE is unacceptable, particularly after servicemembers have fulfilled their commitments.
- Explain the challenges and sacrifices you and your family faced to earn this benefit.
- Highlight the risks associated with cutting TRICARE during a recruiting crisis when our nation is counting on servicemembers and retirees to recommend military service.
MEDIPLUS® TRICARE Supplement
Works hand-in-hand with your Select or Prime Plan. Count on valuable protection.



