Recently, MOAA joined Patrick Grady, the head of the TRICARE program, to hold a second Facebook Live Town Hall event at the Defense Health Agency (DHA). The town hall's focus was on upcoming changes to TRICARE health plans and organizational changes to DHA. The whole event can be viewed below.
The recent town hall generated a lively online discussion. Here are the top questions on the minds of beneficiaries:
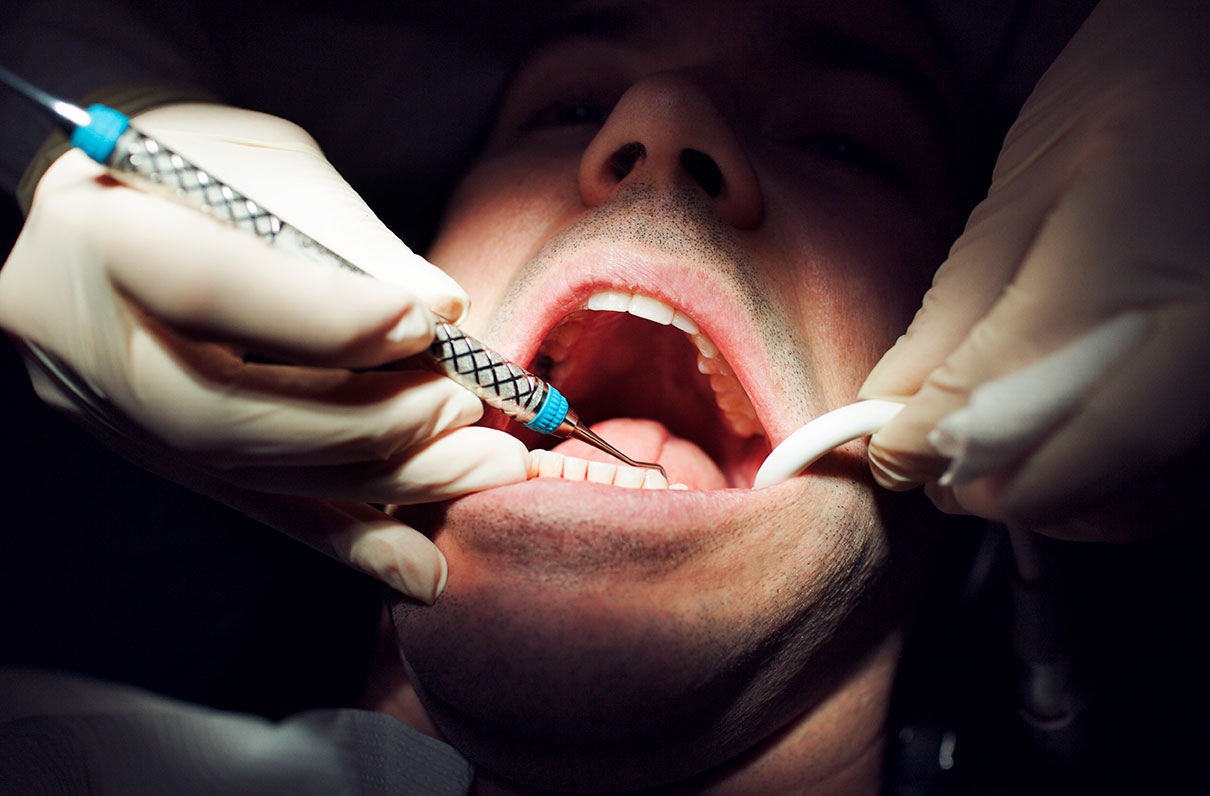
The new dental and vision plans - who, what, where, and when?
Retirees and their family members are eligible to enroll in one of the FEDVIP dental and/or vision plans. Members of the retired reserve, non-active Medal of Honor recipients, and survivors also are eligible to enroll in FEDVIP. For the first time, most active duty family members will be eligible for vision coverage through FEDVIP. If eligible, they may enroll in a plan for self-only, self-plus-one, or self and family coverage. To be eligible for vision coverage, the individual must be enrolled in a TRICARE health plan; this includes TRICARE for Life (TFL).
The current TRICARE Retiree Dental Plan (TRDP) will end Dec. 31, 2018. TRDP members currently using Delta Dental may enroll during the 2018 federal benefits open season (Nov. 12 to Dec. 10) in their choice of FEDVIP dental plans. TRDP enrollees must take action to enroll in a FEDVIP plan to receive dental benefits starting Jan. 1, 2019. When TRDP ends, there will be no automatic enrollment in FEDVIP.
For the latest information, we recommend visiting TRICARE.benefeds.com. Please check back frequently; information such as the established 2019 costs will be updated as it becomes available sometime this fall. Beneficiaries also can sign up to receive alerts when new information is added to the site.
With all of the changes to the TRICARE program, will TFL be affected?
No. Generally, none of the changes to the TRICARE program will affect those beneficiaries enrolled in TRICARE for Life.
Most changes have occurred in the TRICARE Prime and TRICARE Select health plans. However, as described above, the current TRICARE dental plan for all retirees is changing.
Some TFL beneficiaries who receive care at military treatment facilities might also experience changes, as described here.
Why have TRICARE's cost shares gone up so much?
Since Jan. 1, military beneficiaries have experienced unexpected increases in TRICARE fees. These increases resulted from DoD's unilateral decision to change its fee schedules from a percentage-of-cost model to flat-rate fees for TRICARE Select. These structural fee changes disregarded the intention of the 2017 National Defense Authorization Act (NDAA), which said servicemembers and their families would be grandfathered from health care cost-share increases. Both TRICARE Prime and TRICARE Select fees, however, were subject to steep increases.
Of specific interest to beneficiaries were the cost share increases associated with specialty care appointments. For instance, mental health and physical therapy visits are considered specialty care. This change generates significantly higher out-of-pocket costs than under the previous TRICARE Standard or Extra, and they are higher than many civilian plans.
This summer, MOAA members helped to narrowly avert additional steep increases in a Senate-backed proposal in the FY 2019 NDAA. However, the threat of TRICARE fee increases will continue to reemerge in the future.